Finding the best kidney specialist in Bangalore is of utmost importance when it comes to the diagnosis and treatment of kidney-related conditions. Bangalore, known as the hub of healthcare in India, boasts a wide range of medical professionals specializing in nephrology. However, choosing the right kidney specialist can be a daunting task, considering the numerous options available. In this ultimate guide, we will provide you with valuable insights and tips to help you find the best kidney specialist in Bangalore.
Why Choosing the Right Kidney Specialist is Crucial
Selecting the right kidney specialist is crucial for effective diagnosis, treatment, and management of kidney-related conditions. Kidney diseases require specialized care, and a skilled nephrologist can provide you with the necessary expertise and guidance to ensure the best possible outcomes for your kidney health. Additionally, a good kidney specialist will offer personalized care, addressing your unique needs and concerns throughout your treatment journey.
Steps to Find the Best Kidney Specialist in Bangalore
1. Seek Referrals and Recommendations
Start your search by seeking referrals and recommendations from trusted sources such as your primary care physician, family members, or friends. They may have firsthand experience or know someone who has received treatment from a reputable kidney specialist in Bangalore. Gathering recommendations from trusted individuals can help you narrow down your options and provide valuable insights.
2. Research and Gather Information Online
Utilize online resources to research and gather information about kidney specialists in Bangalore. Visit their websites, read their profiles, and explore their areas of expertise. Look for patient reviews and testimonials to gauge the satisfaction levels of their patients. Pay attention to feedback regarding their professionalism, communication skills, and treatment outcomes.
3. Verify Qualifications and Experience
When choosing a kidney specialist, it is crucial to verify their qualifications and experience. Ensure that they are board-certified nephrologists with specialized training in kidney diseases. Check if they have relevant fellowship programs or advanced certifications that demonstrate their expertise in the field. Additionally, consider their experience in treating a wide range of kidney conditions and performing various kidney-related procedures.
4. Consider Hospital Affiliations
Evaluate the hospital affiliations of the kidney specialists you are considering. Look for specialists who are affiliated with reputable hospitals or medical centers known for their excellence in nephrology. A strong hospital affiliation can indicate that the specialist works within a multidisciplinary team and has access to state-of-the-art facilities and advanced treatment options.
5. Assess Communication and Bedside Manner
Communication and a good bedside manner are crucial qualities in a kidney specialist. Consider scheduling a consultation to meet the specialist in person. During this meeting, assess how well they listen to your concerns, explain your condition and treatment options, and address any questions you may have. A compassionate and patient-centric approach is essential in ensuring a positive doctor-patient relationship.
6. Evaluate Patient Satisfaction and Outcomes
Look for indicators of patient satisfaction and treatment outcomes. Check if the kidney specialist has a track record of successful treatments and positive patient experiences. You can inquire about patient outcome statistics or success rates for specific procedures or treatments. Consider the overall reputation of the specialist within the medical community and among their patients.
7. Consider Accessibility and Location
Choose a kidney specialist whose clinic is easily accessible from your location. Consider factors such as proximity to your home or workplace, availability of public transportation, and parking facilities. Accessibility is crucial, especially if you require frequent visits or ongoing treatment for your kidney condition.
8. Verify Insurance Coverage and Financial Considerations
If you have health insurance, it is essential to verify whether the kidney specialist you are considering is covered by your insurance plan. Contact your insurance provider or the specialist’s clinic to ensure that their services are included in your coverage. Additionally, inquire about the specialist’s payment options, including any financial assistance programs or payment plans they offer.
FAQs About Finding the Best Kidney Specialist in Bangalore
1. What is the role of a kidney specialist?
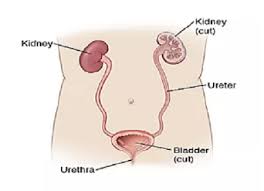
A kidney specialist, also known as a nephrologist, specializes in diagnosing and treating kidney diseases and disorders. They manage conditions such as chronic kidney disease, kidney stones, kidney infections, and kidney failure. They also provide guidance on kidney health maintenance and preventive measures.
2. When should I see a kidney specialist?
You should consider seeing a kidney specialist if you experience symptoms such as persistent high blood pressure, blood in urine, frequent urinary tract infections, or swelling in the hands and feet. Additionally, if you have a family history of kidney disease or have been diagnosed with conditions such as diabetes or hypertension, a consultation with a kidney specialist is advisable.
3. How can I prevent kidney diseases?
To prevent kidney diseases, it is essential to maintain a healthy lifestyle. This includes staying hydrated, eating a balanced diet, exercising regularly, managing blood pressure and blood sugar levels, avoiding excessive use of pain medications, and refraining from smoking.
4. Can I switch kidney specialists if I am not satisfied?
Yes, you have the freedom to switch kidney specialists if you are not satisfied with your current specialist’s services or if you feel another specialist may better meet your needs. However, it is recommended to communicate your concerns and reasons for switching to ensure a smooth transition of your medical records and continuity of care.
5. What questions should I ask during the initial consultation?
During the initial consultation, you can ask questions such as:
– What is the diagnosis for my condition?
– What treatment options are available?
– What are the potential risks and benefits of each treatment option?
– How long will the treatment last, and what can I expect during the recovery period?
– Are there any lifestyle modifications I need to make to manage my kidney condition?
6. Can I receive a second opinion?
Yes, seeking a second opinion is a common practice, especially for complex or serious kidney conditions. It allows you to gain more insights and explore different treatment approaches before making important decisions about your health.
Conclusion
Finding the best kidney specialist in Bangalore requires thorough research and consideration. By seeking referrals, conducting online research, verifying qualifications and experience, evaluating communication skills and patient satisfaction, and considering accessibility and insurance coverage, you can make an informed decision. Remember to prioritize a specialist who not only possesses the necessary medical expertise but also demonstrates compassion, effective communication, and a patient-centric approach. By choosing the right kidney specialist, you are taking a significant step towards the effective management and treatment of your kidney condition.